|
Poor cement coverage and inadequate intrusion into trabecular bone are associated with stem loosening, while deep and uniform penetration is important to the success of total hip arthroplasty.1 Clinical symptoms resulting from loose implants continue to be a significant problem and expose the patient to serious medical risks associated with revision surgery. Current surgical technique for implantation of cemented implants consists of shaping the bony cavity with hand and power tools, followed by brushing and saline lavage. Surgical sponges or tampons are inserted into the cavity to dry the bone surface. The canal is then plugged and cement injected under pressures to assure interdigitation of cement into the prepared cancellous bony bed. Cardiopulmonary dysfunction has been reported as a risk factor associated with the use of cemented arthroplasty. The principal factor is attributed to particulate fat and marrow emboli.2-10 Thorough cleaning of fat tissue and debris helps reduce the incidences of emboli complications.
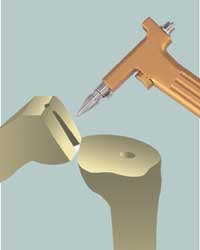
The CO2 lavage system was created for the purpose of using pressurized dry carbon dioxide gas as a lavage to the bony surface, to clean and dry the area prior to cement implantation (Figure 1). Mechanical and clinical investigations of this device have proven it to be safe and effective. The CO2 lavage system is used as the final step in bone preparation, employed immediately prior to cement introduction. The flow of gas aids in removing fat and debris from the bone surface, reducing interposed fluid between cement and bone. The CO2 lavage system consists of a reusable hand piece and a variety of nozzles, along with a pressure regulator needed for use with standard CO2 tanks (Figures 2 and 3). The sterile CO2 tube set features appropriate quick disconnect fittings and an in-line microbial filter for filtration purposes. In vitro testing has been conducted on human cadaver bone to determine impact force as well as cleaning effectiveness as compared to standard pulse saline lavage devices. Results of the laboratory testing demonstrating a significant capability of cleaning and debris removing. In addition, testing demonstrated that a moderate gas flow rate is sufficient to clean and dry the bone. High flow rates have the potential for damaging soft tissue and fragile bony areas. The flowing gas of the CO2 lavage system, however, can be directed at the skin without discomfort or damage to soft tissue. An operating pressure of 50 psi is recommended; the regulator delivery pressure is limited to 65 psi as an absolute maximum. The resulting gas flow rate is approximately 25 lpm. Clinical surgical evaluations demonstrated interoperative monitoring to be uneventful. One-year follow-up monitoring was also uneventful. Throughout the clinical use, no complications have been encountered. Since 1993, and thousands of total joint surgeries, surgical in vivo impressions are that the CO2 lavage system demonstrated improved or equivalent results as compared to pulsating lavage and cleaning cancellous bone prior to cement implantation. Compressed CO2 gas has been employed as an insufflation medium in laparoscopic procedures for many years, and is readily available at all hospitals. Long-term fixation of cemented implants relies on basic mechanical principles of interlocking. Thorough interoperative cleaning of fat, tissue, and debris will help improve long-term fixation while reducing the risk of emboli. Mechanical and clinical testing to date has demonstrated that the use of dry carbon dioxide gas is a safe and effective way of preparing the bone prior to cement implantation and only additional clinical testing and long-term follow-up will determine if the CO2 lavage system can improve long-term clinical outcome results. H. M. Reynolds, MD, is an orthopedic surgeon with the Webster Orthopedic Group, Oakland, Calif, Richard E. Jones, MD, is an orthopedic surgeon with Southwest Orthopedic Institute, Dallas, Tex, and Timothy McTighe, Dr. H.S. (hc), is the executive director and CEO of Joint Implant Surgery & Research Foundation, Chagrin Falls, Ohio.
References
|
|