 Evert J. Smith, MD*; Timothy McTighe, Dr. HS (hc)** Evert J. Smith, MD*; Timothy McTighe, Dr. HS (hc)**
Introduction:
Total Hip Arthroplasty for dysplasia or congenital disease of the hip is technically demanding surgery that requires an in-depth understanding of the complex techniques required to solve the problems of both the pelvis and the femur. It also requires the ability to perform an experienced evaluation of the patient. The ‘high dislocation’ is the extreme example in this range of surgery. Patients are often young or middle aged; their hip pain and functional disability has so adversely affected their quality of life, they are more often than not keen for surgical intervention.
A careful consent pertaining to specific complications related to each individual patient’s pathology is essential, as the surgical solution is not likely to rest with a total hip arthroplasty alone. In the majority of cases, there is often a requirement for treatment of the knees and the thoracolumbar spine as well. Emphasis should be directed toward nerve palsies and the fact that, in the majority of cases, revision surgery will be required.

CDH of the left hip in an elderly person
* Consultant in Trauma and Orthopaedic Surgery and Honorary Clinical Senior Lecturer at the University of Bristol. http://evertsmith.com/
** Executive Director, Joint Implant Surgery & Research Foundation, Chagrin Falls, OH www.jisrf.org Founded in 1971 (Non-Profit)
|
Terminology:
The term ‘developmental dysplasia of the hip’ does not describe the congenital origin of the deformity; nor does the term ‘dysplasia’ describe the variation of the underlying pathology.
Dupuytren observed newborn infants with displacement of the femoral head from the acetabulum and named this condition ‘congenital displacement’. [1] In 1891, Phelps concluded that the majority of such cases are really dislocations in utero or at birth. [2] Anatomy publications and the findings at operation have confirmed the congenital nature of the deformity (Dunn 1976, Howorth 1947, Massie 1958, Massie and Howorth 1951, Ortorlani 1976). [3,4,5,6,7]
Klisic (1989) argued that the term referred to, up until this time, as ‘congenital dislocation of the hip’, was misleading due to variable pathology. [8] A dislocation is not always present.

X-Ray Image Showing Hip Dysplasia in an Infant
Often when dislocation does occur it is in the postnatal period and is therefore not truly congenital. He recommended the term ‘developmental displacement’ and over time this title or description became altered to ‘developmental dysplasia’.
The term ‘dysplasia’ is composed of the Greek words dt1 (bad) and pka9rg (formation). Thus, ‘dysplasia’ could be used for the total spectrum of hip deformities. But, to avoid confusion and diagnostic inaccuracies, it is preferable for the term to be reserved for the milder types of hip deformities. Terminology covering the entire pathology of congenital deformities of the hip (or a generally accepted classification of its types), which will improve our communication, treatment planning, and evaluation of results of treatment, is often inaccurate.
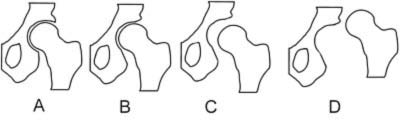
Types of misalignments of femoral head to the socket in hip dysplasia [9]
A: Normal B: Dysplasia C: Subluxation D: Luxation
Gaston et al in 2009 published a reliability study arguing that in their opinion the Crowe and Hartofilakidis classifications did not predict the surgical difficulties they encountered when performing surgery on this group of patients. Their classification describes the femur and the acetabulum separately. The acetabulum is divided into: AI - the dysplastic acetabulum. AII - the acetabulum associated with low femoral dislocation. AIIIa - the post-surgical acetabulum with metalwork. AIIIb - without metalwork in-situ. [10]
The femur is classified as: F1 - dysplastic but contained within a true or low acetabulum. FII - the high femur. FIIIa - the post-surgical femur with metalwork. FIIIb - the post-surgical femur without metalwork in-situ. This classification emphasises the surgery that may be required on the femur and reminds the surgeon of previous surgery to both the pelvis and the femur. It showed inter- and intra- observer reliability, comparable to that of the Crowe and Hartofilakidis classification. It should be emphasised that the more severe the anatomical derangement, the less chance of long term survival of the total hip arthroplasty (Chougle et al 2005, Hartofilakidis et al 2004). [12,13]
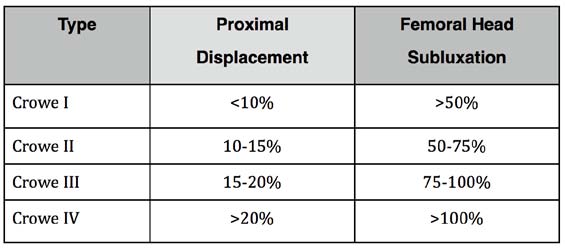
Crowe Classification [11]
Despite the various classifications used in different orthopaedic centres, the outcome is ultimately dependent on the experience and skill of the surgeon performing surgery on dysplasia and congenital dislocation of the hip. Clearly the surgeon must take into account all the anatomical distortions of the pelvis and femur, as well as the derangement and alteration of the surrounding soft tissue. In the more severe cases it is important to perform 3D CT scans to aid one in the algorithmic approach to the management of these patients.
Studies:
In cemented total hip arthroplasty (THA), a number of studies have postulated that a high hip centre or a lateralised centre of rotation (COR) adversely affects the longevity of cups in normal (Hirakawa et al 2001, Pagnano et al 1996) [14,15] and dysplastic hips (Iida et al 2000, Hartofilakidis et al 1996, Stans et al 1998). [16,17,18] In one study, shifting the COR more than 5mm superiorly or laterally accelerated aseptic loosening of the stem and peri-acetabular osteolysis (Hartofilakidis et al 1996). [17]
In another publication, lateralisation of the COR was the most significant factor associated with radiographic signs of loosening (Karachalios et al 1993). [19] Similarly, with cementless cups, it has been reported that shifting the COR superiorly or laterally was the most important variable associated with aseptic loosening in DDH (Georgiades et al 2010). [20]
A long-term study of cemented THAs with a mean follow-up of 12.3 years (8 to 24 years) showed a 96% survival of the acetabular component at 15 years, with revision for aseptic loosening. Survivorship of 75% was noted when radiological loosening was used. Risk factors for loosening were identified as trochanteric non-union, lateral placement of the socket and delayed trabecular reorientation of the bone graft (Iida et al 2000). [20]
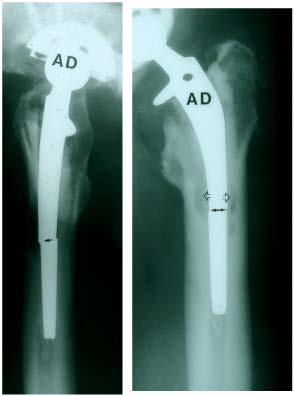
Fractured stem
Cameron and McTighe reported on 262 CDH cases from 2-18 year results at the Combined Scientific Meeting for the AOA and NZOA in 2006 and demonstrated that cement in the femoral canal does poorly when the stem is small interfacing with a thin cement mantle. Often you are required to ream heavily to get a cemented stem in, so most of the cancellous bone is gone resulting in a poor cement interlock. [22]
The capacity to alter version is very limited in small canals. In CDH cases a large amount of anteversion may have to be accepted which can result in a post-operative toe-in gait. This condition can lead to frequent falls.
In 2009, a report from the University of Athens Medical School, on a cohort of patients with DDH using cemented THAs, with a minimum 22-year follow-up, documented that 37 (44%) of 84 hips had failed. In 32 hips, 28 acetabular and 30 femoral components were revised because of aseptic loosening; 6 of the loose femoral components were broken. Three hips were infected and converted to a resection arthroplasty, while periprosthetic femoral fractures occurred in two additional hips (Georgiades et al 2009). [22]

Distal stem fixation can also result in a cantilever effect resulting in stem failure.

Proximal load transfer will reduce this cantilever effect. (Cameron)
Intermediate follow-up studies using hybrid THAs have reported good results at an average follow up of 10.6 years. Structural allograft was used in 15 of the 100 hips in their cohort of patients. Revisions were performed in 2 hips due to recurrent dislocation. The Kaplan-Meier survivorship analysis, with failure defined as revision surgery, demonstrated that the probability of retention of the acetabular component 15 years after surgery was 98% and that of the femoral component was 100% (Ito et al 2003). [23]
In a study of 56 THAs in patients with DDH, using cementless Harris-Galante type-I cups with structural grafting and cemented stems, the authors reported on 53 of the surviving patients. After an average duration of 10.2 ± 2.9 years, 4 implants had been revised and 2 had radiographic evidence of loosening. Using revision and loosening as end points, the 11-year survival rates were 91.6% and 88.9%, respectively. Of the 50 implants that had no loosening, 14 had measurable cup migration, 35
had no migration, and 1 implant could not be measured. All migrations except one were progressive. With loosening used as the end point, the survival rate at 11 years was 100% for the implants with no migration; however, the survival rate for the cups that had migrated was 69.3% (Hendrich et al 2006). [24]
In another study of 35 patients with a follow-up of 7.5 years (range 5 - 12.3 years), a cementless porous-coated titanium cup fixed with screws and autogenous bulk femoral head graft was used. The survival of the acetabular component at 7 years was 92.6% with revision for aseptic loosening. Forty-one of the 44 femoral stems were cementless - 7.4% were revised; 2 hips for severe polyethylene wear and osteolysis, 1 for aseptic loosening and 1 for breakage of the acetabular shell (Spangehl et
al 2001).[25]
In a publication where the follow-up was short (3 to 5 years), the authors used a cementless stem, specifically designed for use in DDH patients. The straight titanium alloy stem had a collar and a wedge shape of 3 degrees. The proximal third was porous-coated, and oval on section. The neck angle was 135 degrees and the offset of the stem varied from 31 to 39 mm. Loosening of the femoral stem occurred in 4 hips, 3 of which resulted from the same technical error. The greater trochanter had been detached so far distally, that the lateral support of the stem was insufficient to provide reliable rotational stability. The fourth loosened stem was small and lacked rotational stability. A 50% failure was documented with their smooth-threaded cup (Paavilainen et al 1993). [26]
In another study, 80 hips with severe acetabular dysplasia (Crowe grades III and IV) were reviewed. In 32 hips, over 20% of the cup was not covered by the acetabulum and was reconstructed with a femoral head graft. In the second sub-group of 48 hips, graft was not used as the socket was adequately covered. The mean follow-up period was around 9 years (range 3–18 years). Early complications were frequent (19%). Early cup loosening was more frequent in adequately covered sockets. Acetabular cup loosening did not correlate with acetabular cup position. Bone-graft appeared consolidated in all cases, but resorption areas were frequently observed. In 78 hips with follow-up, grafted hips showed good results in 69.6% after 16 years, compared with those hips with bone coverage (52.2%). However, there was no significant difference between the groups (Garcia-Cimbrelo and Munuera 1993). [27]
Deviation from the optimal COR when positioning the cup will adversely influence hip loads, bearing surface wear and ultimately implant survival (Bicanic et al 2009, Denham 1959, Johnston et al 1979). [28,29,30] Increasing the femoral neck length and lateral offset appear beneficial in reducing hip load (Johnston et al 1979). [31]
The Pelvis
At one end of the spectrum of DDH the socket may be slightly shallow, the centre edge angle of Wiberg is decreased and the extrusion index is increased (Wiberg 1939). [32] The angle of Sharp is altered and as the dysplasia becomes more pronounced, the acetabulum becomes shallower, sloped and less hemispherical (Sharp 1961). [33] In lower dislocations, the diameter of the acetabular socket is increased from superior to inferior and the medial wall of the acetabulum becomes redundant. In high dislocations, the acetabular socket is false. The anteversion of the socket increases and the original foetal socket is rudimentary, reduced in size from lateral to medial and filled with fatty fibrous tissue. By this stage the anterior wall is thinned, porotic and is often residual.
In a false acetabulum, the lever arm for body weight is much longer than the abductors, leading to excessive load. The shearing forces acting on the acetabular cup may lead to early loosening. Abductor insufficiency, leg length discrepancy and limp are reduced when the true or anatomical socket is used (Karachalios et al 1993). [34]
The strongest and most viable bone for use is at the original socket. I always try and restore the true centre of rotation in the original socket. The involved hemi-pelvis is usually smaller than the contralateral hemi-pelvis. However, one is always able to find the true floor by identifying the fatty tissue at the base of the socket. The transverse ligament and the inferior border of the true acetabulum are key landmarks.
Several acetabular socket reconstruction techniques, aimed at improving osseous coverage and support for cemented or cementless cups, have been reported. These include: augmentation of the superolateral margin of the acetabular rim with bulk autograft (Harris et al 1977); [35] superior positioning of the acetabular cup to create a high hip centre (Russotti et al 1991); [36] medialization of the hip centre by the cotyloplasty technique (Dunn and Hess 1976, Hartofilakidis et al 1996) [37,38] or the protrusion socket technique (Dorr et al 1999); [39] impaction grafting (Somford et al 2008); [40] additional use of a reinforcement ring (Gill T et al 1998); [41] or using small diameter cementless or cemented cups alone (Jasty et al 1995). [42] Various methods of acetabular cup fixation are used to optimize the outcome and long-term survival in patients with a ‘high dislocation’.
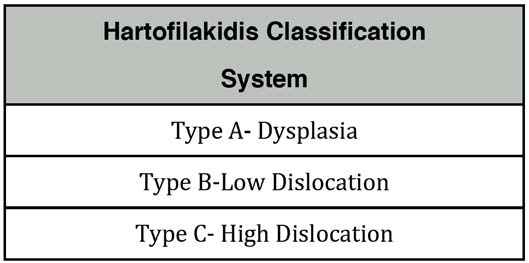
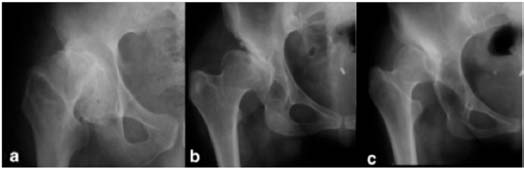
Type A, Type B, Type C
A - The femoral head is contained within the original acetabulum.
B - The femoral Head articulates with a false acetabulum that partially covers the true acetabulum.
C - The femoral head is migrated superiorly and posteriorly to the hypolastic true acetabulum.
In the dysplastic hip and in patients with a ‘low dislocation’, we use the Exceed ABT 15° Face Changing cup (15°FC) (Biomet UK).

The design modifications of the Exceed ABT 15° face changing acetabular cup will alter the surgical strategy and treatment of secondary osteoarthritis in patients with shallow acetabular sockets in the future.
The unique design feature of this acetabular cup adjusts the bearing surface, closing the inclination angle by 15° and allows for optimisation of the ceramic liner which is a significant advantage in this group of patients.
The standard ‘directional’ reaming technique is modified to perform progressive reaming with the face of the reamer directed parallel to the face of the dysplastic socket (not at 40° abduction or inclination). Typically, when completed, the rim of the final reamer is flush to the acetabular rim, aligned at 50-60° inclination and 15-20° anteversion.
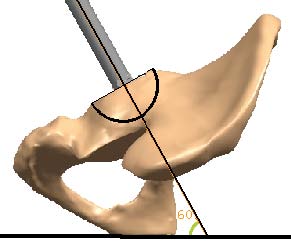
60º inclination & 15-20º anteversion
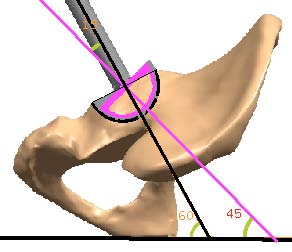
The 15°FC hemispherical porous coated cementless shell is introduced in the same axis as the reamer (introducer at 50-60° abduction and 15-20° anteversion) to ensure the cup’s liner is in the optimal position of 35-45° inclination and 15-20° anteversion (inclination 15° less than the hemispherical shell and introducer) with the porous coated surface of the cup achieving full coverage and host bone contact.
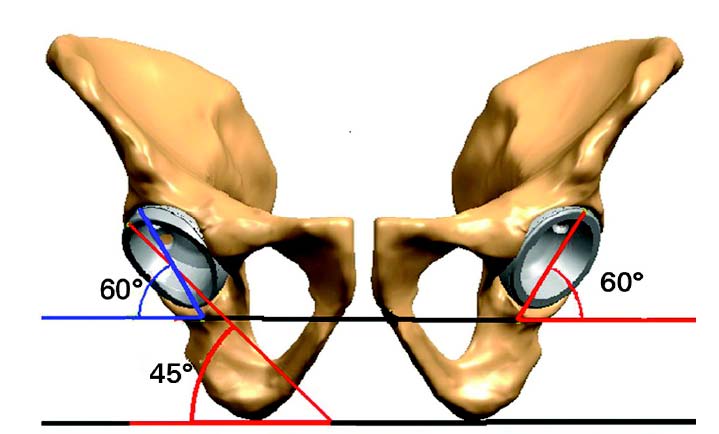
Left: diagram showing the 15° face-changing cup in the optimal position, with a cover angle with the liner of 60° (in blue), and a face-changing angle with the liner of 45° (in red). Right: diagram showing a 'standard' component incorrectly positioned at a high inclined angle of 60° to obtain full contact with host bone.
The cup may require supplementary screws for fixation of the shell, after removal of the blanks from the chosen screw holes, followed by insertion of the appropriate size ceramic liner.
The appropriate positioning of the acetabular implant and alignment of the bearing surface can be reliably achieved with the 15°FC cup in ‘dysplasia’ and ‘low dislocation’ DDH. Furthermore, the 15°FC cup eliminates the need for acetabular augmentation with femoral head autograft or bulk allograft, the use of which has been associated with reduced THA survival (Mulroy et al 1990, Shinar et al 1997). [44,45]
Inclination higher than 45° is associated with a higher rate of wear, irrespective of the type of bearing surface.
The Femur
In general, there is an increased caput collum diaphysis (CCD) angle and obvious coxa valga in the ‘dislocated hip’. The proximal femur is anteverted and the greater trochanter is positioned posteriorly. The femoral head is small and the femoral neck is foreshortened and mildly anteverted. In the metaphysis and proximal diaphysis there is a reduction in size.

Small femoral head with shortened neck and mildly anteverted.
The distortion of the anatomy is more often than not associated with abductor deficiency and a leg length discrepancy; the leg is foreshortened, as well as being reduced in size. In ‘high dislocation’ the abductor function is nonexistent, accounting for the waddling gait. There is often associated thoracolumbar curvature in relation to the leg length discrepancy. It is therefore not uncommon that this group of patients present with lower back pain.
Operation
All cases are performed with a modified Kocher Langenbeck approach. The pelvic bone is marked by a pin in the iliac crest and osteotomy notches are made in the metaphysis and in the diaphysis, at marked points on the bone cortex, to increase the accuracy of bone resection. Care must be taken to minimise periosteal stripping.
The tension on the sciatic nerve with leg lengthening is critical. The sciatic nerve is always identified through the posterior approach and the tension of the nerve palpated at the beginning of the operation. The tactile feel of the tethering and tightness of a ‘guitar wire’ feel in the nerve should be noted as the leg is lengthened. An iliopsoas release and partial abductor release is nearly
always required in the more complex hip. A subcutaneous adductor tenotomy can be performed if this is restrictive.
When performing surgery on the acetabulum with the 15°FC cup it is not necessary to perform graft fixation. If the socket is too small to utilise the face changing method, then alternative acetabular cups are utilised and block graft from the femoral head is fixed with K wires and reamed to allow optimum positioning of the cup followed by definitive fixation of the graft with screws.
If the bone is osteoporotic and weak, it may require seating of the acetabular component deep to the floor. The central part of the floor can be incised to allow the dome of the cup to breach the socket floor. Impaction bone grafting is used and placed in the true floor and milled bone chips are used liberally in the socket as required.
In ‘high dislocations’, a trochanteric osteotomy is performed as this allows access to the socket, not only for preparation of the socket, but it also
allows a clear run at further resection around the proximal femur and for trialing of the stems available for the procedure.
Distal advancement of the trochanter is required, with fixation of the greater trochanter, using an impaction mesh and wires and/or screws, or screws and a plate. A low profile trochanteric grip and plates with cables can simplify the technique in some cases.
Fixation of the trochanter is performed with the hip in extreme abduction. The anterior portion of vastus lateralis may require release. Central tightness of the gluteus medius may also require partial release in order to distalise the trochanter far enough to stabilise it onto the proximal femur.
Placing the stem through the proximal femur and then moving the femur from an abducted position into an adducted position allows the surgeon to visually estimate if further excision of the femur is required. This should be performed in a step-wise manner until reduction of the head in the socket is possible (Masonis et al 2003, Park et al 2007, Crych et al 2009). [46,47,48]
Using these techniques, and by careful surgery, the leg can be lengthened up to 2-3 centimetres in some hips. Collarless straight stems with a varus neck shaft angle, long stems or customised stems, can be used when standard stems do not allow insertion into the femoral canal.
The intramedullary canal may require reaming to widen it in order to achieve fixation of the femoral stem. Given the type and style of stem, an osteotomy to split the femur longitudinally may also be required. If the cementless stem has distal grip and rotational control, then cortical fixation of the femur may not be required.
The wound is closed in sequential layers, more often than not without a wound drain.
Rehabilitation
The patient is usually mobilised full weight bearing on day one or two following check radiographs. All patients require physiotherapy to gently stretch the abductor musculature. Patients with osteotomised femurs are mobilised partial weight bearing, steadily increasing the range of hip movement in flexion, extension, abduction and adduction but avoiding flexion and internal rotation to extremes. By six weeks, exercises can be initiated against resistance and full weight bearing.
‘High dislocation’ patients often require crutches for a period of 3 months as the abductor muscle strength is increased and the limp and waddling gait is eliminated.
- Dupuytren G. The Classic: Original or congenital displacement of the head of thigh-bones. Clin Orthop Relat Res. 1964; 33: 3–8
- Phelps AM. The Classic: Congenital dislocation of the hip. Clin Orthop Relat Res. 2008; 466: 763–770
- Dunn PM. The anatomy and pathology of congenital dislocation of the hip. Clin Orthop Relat Res. 1976; 119: 23–27
- Howorth MB. Congenital dislocation of the hip. Ann Surg. 1947; 125: 216–236
- Massie WK. Congenital dislocation of the hip - its causes and effects. Clin Orthop Relat Res 1958 ; 8: 103–121
- Massie WK, Howorth MB. Congenital dislocation of the hip. Part III: Pathogenesis. J Bone Joint Surg Am. 1951; 33: 190–198
- Orlorani M. The Classic: Congenital hip dysplasia in the light of early and very early diagnosis. Clin Orthop Relat Res. 1976; 119: 6–10
- Klisic PJ. Congenital dislocation of the hip: a misleading term. J Bone Joint Surg Br. 1989: 71: 136
- Londenp, Schematic depiction of hip joint structures’ positions in hip dysplasia. Oct. 8, 2006, http://en.wikipedia.org/wiki/File:Hip_dysplasia_-_schematic.jpg
- Gaston MS, Gaston P, Donaldson P, Howie CR. A new classification system for the adult dysplastic hip requiring total hip arthroplasty: a reliability study. Hip Int 2009; 19: 96-101
- Crowe JF, Mani VJ, Ranawat CS (1979). “Total hip replacement in congenital dislocation and dysplasia of the hip”. J Bone Joint Surg Am 61 (1): 15–23. PMID 365863.
- Chougle A, Hemmady MV, Hodgkinson JP. Severity of hip dysplasia and loosening of the socket in cemented total hip replacement. A long-term follow-up. J Bone Surg 2005; 87: 16-20.
- Hartofilakidis G, Karachalios T. Total hip arthroplasty for congenital disease of the hip. J Bone Joint Surg Am. 2004; 86: 242–250
- Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res 2001; 388: 135-4218
- Pagnano W, Hanssen AD, Lewallen DG, Shaughnessy WJ. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am 1996; 78:1004-1014
- Iida H, Matsusue Y, Kawanabe K, Okumura H, Yamamuro T, Nakamura T. Cemented total hip arthroplasty with acetabular bone graft for developmental dysplasia: LONG-TERM RESULTS AND SURVIVORSHIP ANALYSIS, J Bone Joint Surg (Br) 2000; 82: 176-184
- Hartofilakidis G, Stamos K, Karachalios T, Ioannidis T Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg 1996; 78: 683-692
- Stans AA, Pagnano MW, Shaughnessy WJ, et al. Results of total hip arthroplasty for Crowe Type III developmental hip dysplasia. Clin Orthop Relat Res 1998; 348:149-157
- Karachalios T, Hartofilakidis G, Zacharakis N, Tsekoura M. A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty. The role of the center of rotation. Clin Orthop Relat Res 1993; 296:140-147
- Georgiades G, Babis GC, Kourlaba G, Hartofilakidis G. Effect of Cementless Acetabular Component Orientation, Position, and Containment in Total Hip Arthroplasty for Congenital Hip Disease. J Arthroplasty 2010; 25:1143-1159
- Iida H, Matsusue Y, Kawanabe K, Okumura H, Yamamuro T, Nakamura T. Cemented total hip arthroplasty with acetabular bone graft for developmental dysplasia: LONG-TERM RESULTS AND SURVIVORSHIP ANALYSIS J Bone Joint Surg (Br) 2000; 82: 176-184
- Cameron, H.U., McTighe, T. Long-Term Results in CDH THA. Oral Paper Combined Scientific Meeting AOA & NZOA, Oct. 2006, Canberra, Australia Georgiades G, Babis GC, Hartofilakidis G. Charnley. Low-Friction Arthroplasty in Young Patients with Osteoarthritis - Outcomes at a Minimum of Twenty-two Years. J Bone Joint Surg 2009; 91: 2846-2851
- Ito H, Matsuno T, Minami A, Aoki Y. Intermediate-term Results After Hybrid Total Hip Arthroplasty for the Treatment of Dysplastic Hips. J Bone Joint Surg 2003; 85: 1725-1732
- Hendrich C, Mehling I, Sauer U, Kischner S, Martell JM. Cementless Acetabular Reconstruction and Structural Bone-Grafting in Dysplastic Hips. J Bone Joint Surg 2006; 88: 387-394
- Spangehl M, Berry D, Trousdale R, Cabanela Miguel E. Uncemented Acetabular Components with Bulk Femoral Head Autograft for Acetabular Reconstruction in Developmental Dysplasia of the Hip : Results at Five to Twelve Years. J Bone Joint Surg 2001; 83: 1484-89
- Paavilainen T, Hoikka V, Paavolainen P. Cementless total hip arthroplasty for congenitally dislocated or dysplastic hips. Clin Orthop 1993: 297: 71-81
- Garcia-Cimbrelo E, Munuera L. Low-friction arthroplasty in severe acetabular dysplasia. J Arthroplasty 1993; 8: 459-469
- Bicanic G, Delimar D, Delimar M, Pecina M: Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop 2009; 33: 397-402
- Denham RA. Hip mechanics. J Bone Joint Surg Br 1959; 41:550-57.
- Johnston RC, Brand RA, Crowninshield RD. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am 1979; 61: 639-52
- Johnston RC, Brand RA, Crowninshield RD. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am 1979; 61: 639-52
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand 1939; 83 (Suppl ):58
- Sharp IK. Acetabular dysplasia The acetabular angle . J Bone Joint Surg 1961; 43: 268-272
- Karachalios T, Hartofilakidis G, Zacharakis N, Tsekoura M. A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty. The role of the center of rotation. Clin Orthop Relat Res 1993; 296:140-147
- Harris WH, Crothers O, Oh I. Total hip replacement and femoral-head bone-grafting for severe acetabular deficiency in adults. J Bone Joint Surg 1977; 59: 752-59
- Russotti GM, Harris WH. Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study. J Bone Joint Surg 1991; 73:587-92
- Dunn HK, Hess WE. Total hip reconstruction in chronically dislocated hips. J Bone Joint Surg Am 1976; 58:838
- Hartofilakidis G, Stamos K, Karachalios T, Ioannidis T Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg 1996; 78: 683-692
- Dorr LD, Tawakkol S, Moorthy M, Long W. Medial protrusio technique for placement of a porous-coated, hemispherical acetabular component without cement in a total hip arthroplasty in patients who have acetabular dysplasia. J Bone Joint Surg 1999; 81: 83-92
- Somford MP, Bolder SBT, Gardeniers JW, Slooff TJJ, Scheurs BW. Favorable Survival of Acetabular Reconstruction With Bone Impaction Grafting in Dysplastic Hips, Clin Orthop and Relat Res 2008; 466: 359-365
- Gill T, Sledge JB, Muller ME. Total hip arthroplasty with use of an acetabular reinforcement ring in patients who have congenital dysplasia of the hip. Results at five to fifteen years. J Bone Joint Surg 1998; 80: 969-79
- Jasty M, Anderson MJ, Harris WH. Total hip replacement for developmental dysplasia of the hip. Clin Orthop Relat Res 1995; 311: 40-45
- C. K. Yiannakopoulos,1,4 T. Xenakis,2 T. Karachalios,3 G. C. Babis,1 and G. Hartofilakidis1. Int Orthop. 2009 April; 33(2): 353–358. Published online 2007 November 6. doi: 10.1007/s00264-007-0472-0
- Mulroy RD, Harris WH. Failure of acetabular autogenous grafts in total hip arthroplasty. Increasing incidence: a follow-up note. J Bone Joint Surg 1990; 72: 1536-1540
- Shinar AA, Harris WH. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg 1997; 79: 159-68
- Masonis J, Patel J, Miu A, Bourne R, McCalden R, MacDonald S, Rorabeck C. Subtrochanteric shortening and derotational osteotomy in primary total hip arthroplasty for patients with severe hip dysplasia: 5-year follow-up. J Arthroplasty 2003; 18: 68-73
- Park M, Kim K, Jeong W. Transverse Subtrochanteric Shortening Osteotomy in Primary Total Hip Arthroplasty for Patients With Severe Hip Developmental Dysplasia J Arthroplasty 2007; 22: 1031-1036
- Krych A, Howard J, Trousdale R, Cabanala M, Berry D. Total Hip Arthroplasty with Shortening Subtrochanteric Osteotomy in Crowe Type-IV Developmental Dysplasia. J Bone Joint Surg 2009; 91: 2213-2221
|

