Information for Patients of Total Hip Replacement, or Total Hip Arthroplasty (THA)
What is Total Hip Replacement?
 Bechtol and many others have described this as one of the most exciting surgical advances since the 1960’s. It culminates years of research by orthopedic surgeons, biomechanical engineers, and material technologists. Bechtol and many others have described this as one of the most exciting surgical advances since the 1960’s. It culminates years of research by orthopedic surgeons, biomechanical engineers, and material technologists.
The hip joint is a ball-and-socket joint created by the articulation of the head (ball) of the femur with the concave surface (socket) of the acetabulum. Total Hip Arthroplasty is the surgical treatment that replaces the natural bony articulations with artificial implants. There are approximately 200,000 Total Hip Replacements (THR) performed in the United States per year. Needless to say, this has become a common treatment modality replacing the older procedures of arthrodesis (fusion) and osteotomy.
 |
 |
| Example of hip socket worn out |
Example of damaged femoral head |
Indications for THA are for sever pain and /or disabled joint motion caused by a variety of diseases, deformities and/or trauma. Contraindications are active local or systemic infections, loss of musculature, neuromuscular compromise or vascular deficiency in the affected limb and/or poor bone quality.
In addition to contraindications the following conditions tend to adversely affect hip implants: excessive patient weight, high levels of patient activity, likelihood of falls, poor bone stock, metabolic disorders, and disabilities of other joints. The following are the most frequent adverse events after THA: change in implant position, loosening or fracture of implant, dislocation, infection and tissue reaction.
Since the introduction of the total hip arthroplasty the question of how long implant parts could be expected to function in daily use has been of concern to those involved, especially the patient. The results from mechanical wear simulators, material test and laboratory evaluations notwithstanding, only the passage of time (years) have allowed the orthopaedic community to project with some degree of confidence the expected service life of the total hip replacement.
The human body is mechanically complex and subjects the hip joint to great forces. Many studies have demonstrated that the resultant loads on the femoral head during activity are several times higher than body weight.
Hip joint load is a function of body weight, activity level, muscular force, and the distance from the body’s center of gravity to the center of the femoral head. Publications have stated that the hip joint force increases up to 2.5 times body weight with speed in level walking. Considerable forces in all axes were also associated with hip flexion from a supine position, which demonstrated that weight bearing is not essential for the generation of large forces through the hip joint.
Estimates on patient activity during the 1970s-80s were about 1 million cycles per year. Current papers are estimating as high as 10 million cycles per year with increased impact loads. There is no question that more research is needed to predict what types of activities patients can experience without putting at risk their reconstruction. As history has demonstrated, fatigue failure has been with us from the beginning of total hip arthroplasty and there is no indication that it will not be a significant problem for years to come.
Total Hip Components
- The total hip replacement consists of a number of major components that are permanently implanted in the body.
- The socket “cup” replaces the damaged acetabulum. This device can be fabricated in a variety of designs and materials.
- The surgeons decide by their training and experience what style and material are best for each patient and their life style.
- Some of their choices are
- Type of bone fixation (cement or cementless)
- Type of bearing material: (metal on plastic, metal on metal, ceramic on plastic, ceramic on ceramic)
 |
 |
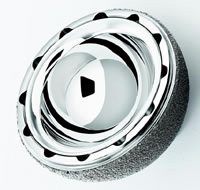 |
| Example of cementless ceramic on ceramic bearing with a cementless cup |
Example of ceramic head on poly socket cementless porous cup. |
Example of metal cup bearing surface |
Note: There is ongoing research on new materials for bearing surfaces such as ceramic on metal, diamond on diamond, etc.
The stem replaces the femoral head and articulates with the socket. The component also is available in a variety of designs and materials. The stem can be fixed to the femoral host bone by either the use of bone cement or of cementless fixation by press fit or porous ingrowth materials. Most modern day stem devices feature a modular head and some of the newer designs also feature a modular neck or proximal body that provide additional benefits that enable the surgeon to reconstruct proper mechanics of the hip joint.
 |
 |
 |
| Cross section of metal modular femoral head. |
Metal femoral head. |
Ceramic modular femoral head. |
It is easy for patients to get confused due to the variety of design and material selection now available for surgery. Often patients talk with one another and ask what their friend had implanted in them. It is important to remember that the selection process is the responsibility of their surgeon and often that surgeons will use different devices for different patient profiles and related activities. There is no one single right answer or choice. Just because a surgeon used one choice that does not mean, if the same surgeon or a different surgeon did not use this selection on you that he used the wrong device.
 |
 |
 |
 |
| Example of monoblock cementless femoral stems (1990) |
Example of proximal modular cementless femoral stem (2003) |
Example of cemented modular proximal stem. (2000) |
Bechtol hip from 1970. |
Implant selection is a comprehensive and complex decision making process. The goal is to provide the individual patient with options that fit their needs. It is only prudent that patients be informed and participate in the decision making process.
Adding to patients’ confusion is surgical approach into the hip joint. Today with the Internet and direct advertisement by hospitals, doctors and corporations there is more information available to the patient than ever before. However, having the ability to interpret all this information at times can be quite difficult.
Surgical Approach
Surgical approach means what surgical incision the surgeon uses to enter the hip joint. Again this is the decision of your surgeon and is based on his training, experience and specific indications for each individual patient.
| The anterior-lateral approach |
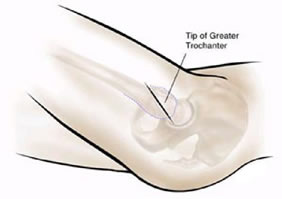 |
| The posterior approach |
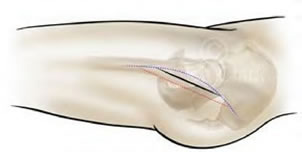 |
| Two-incision anterior approach |
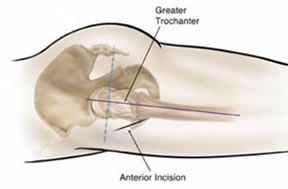 |
There are even variations of these incisions created by individual surgeons.
 |
 |
| Minimal Invasion Incision using the posterior approach of Dr. Lawrence D. Dorr |
Example of Professor Kristaps J. Keggi Dual Muscle Sparring Approach |
JISRF Recommendations
  Patients should be careful in their selection of surgeon this is the single most important decision the patient can and will make. Also, be aware that we are facing a technological boom in the medical field and in particular the orthopedic surgical field of medicine. There are trends in the field of medicine that at times unduly influence patients. Patients should be careful in their selection of surgeon this is the single most important decision the patient can and will make. Also, be aware that we are facing a technological boom in the medical field and in particular the orthopedic surgical field of medicine. There are trends in the field of medicine that at times unduly influence patients.
JISRF suggest to all potential patients of total hip and total joint surgery that they seek highly trained total joint specialist. Some credentials to look for are:
- Orthopaedic Board Certified Surgeons
- Fellowship Trained Total Joint Surgeons
- Members of the American Association of Hip & Knee Surgeons
There are a number of sites that provide additional information for orthopedic patients. For more information please visit our Related Sites page.
References
- Pearl, R. E., et al, “ Biomechanics and Pathomechanics of the Hip”, The Art of THA by Grune & Stratton, Inc.
- Greenwald, S.A., et al, “Biomechanics of the Reconstructed Hip”, Ortho Clin North Am 4:435-447, 1973
- Paul, J.P.,” Load actions on the human femur during walking and some stress resultants” , Exp Mech 192BR: 121-125, 1971
- Paul, J.P., “Force actions transmitted by joints in the human body”, Proc R Socv Lond (Bio) 192B:163-172, 1976
- Rybick, E.F., et al, “On the mathematical analysis of stress in the human femur”, J Biomech 5:203-215, 1972
- Rydell, N., “Intravital measurements of forces acting on the hip joint”, in Evans FG (ed) Studies on the Anatomy and Function of Bone and Joints. New York, Springer-Verlag, 1966, pp 52-68
- Scheller, A.D., et al, “Hip biomechanics and prosthetic design and selection”, in Turner, R.H., Scheller, A.D., (eds): revision Total Hip Arthroplast, Orlando, Fl: Grune & Stratton, 1982
- Willert, H.G., et al, “Clinical experience with Mueller total hip endoprostheses of different designs and materials”, in Hastings, G.W. Williams DF (ed): Mechanical Properties of Biomaterials. New York, John Wiley & Sons, 1980, pp 85-101
- Williams, J.F., et al, “ A force analysis of the hip joint”, Biomed Eng 3:365-370, 1968
- Buch, J.D., et al, “Biomechanical and biomaterial considerations of nature teeth, tooth replacements, and skeletal fixation”, J of Biomaterials, Medical devices and artificial Organs 2-2:171-186, 1974
- Bechtol, C.O., “ Failure of Femoral Implant Components In Total Hip Replacement Operations”, Ortho Review Vol IV Number XI 1975
- Clark, I.C., et al “ Finite Element Analyses Studies of Total Hips Versus Clinical Reality”, International Conference on Finite Elements in Biomechanics, Sponsored by The National Science Foundation & The University of Arizona College of Engineering, 1980
- Collis, D.K., “Cemented total hip replacement in patients who are less than fifty years old”, J. Bone and Joint Surg., 66-A: 353-359, March 1984
- Schulte, K.R. et al, “The outcome of Charnley total hip arthroplasty with cement after a minimum twenty-year follow-up.” The results of one surgeon. J. Bone and Joint Surg., 75-A:961-975, July 1993
- Charnley, J., “Low Friction Arthroplasty of the Hip” Springer-Verlag 1979
- McTighe, T., et.al, “Design Consideration for Cementless Total Hip Arthroplasty” Encyclopedic Handbook of Biomaterials and Bioengineering, Marcel Decker, 1995
- Stauffer RN: “Ten- year follow-up study of total hip replacement” J Bone Joint Surg 64A:983-999, 1982
- Sutherland CJ, et al “Ten-year follow-up of one hundred consecutive Muller curved-stem total hip arthroplasties” J Bone Joint Surg 64A:970-982, 1982
- Davies, J.P., et al, “ Comparison of the Fatigue Characteristics of Centrifuged and Uncentrifuged Simplex P Bone Cement”, J Ortho Research 366-371, 1987
- Hip Implant Price Comparison, 2004 Orthopaedic Network News
- Amstutz, HC. Clin Orthop Rel Res 170:21, 1982
- Reynolds, et al, “ New Approach for Preparation of Boney Surfaces for Cemented Total Joint Arthroplasty, JISRF Update, Nov 2001
- Oh, I. et al, “ A Cement Fixation System for Total Hip Arthroplasty” Clin Ortho, April 1982, Vol 164
|
