 Louis Keppler, MD* and Timothy McTighe, Dr. HS (hc)** Louis Keppler, MD* and Timothy McTighe, Dr. HS (hc)**
 Modular Head
Modular Head |
Abstract:
Every few years there are concerns raised regarding modular junctions and related findings as to fatigue failure, pseudo tumors, surface corrosion[5,6,7], and metallosis.[1,2,3,4]
This has not been our experience with the use of modular stems. Modular stem means that the stem has two or more parts that are connected by a mechanical junction. Almost all hip stems today feature a modular head, however that does not meet the current definition of a modular stem. This paper is a review of the senior surgeon's practice based in two community hospitals and his experience with four different stem styles and three different modular junctions. The S-Rom® Stem[8,9,10,15], Apex Modular11 Stem™, Apex K2 Modular[32] Stem™ and The Apex ARC™ Modular Stem[16].
Since 1986 until May 2012 a total of 1,114 modular stems have been implanted for Primary Total Hip Arthroplasty. To-date there has been no failures of any modular junctions. No fatigue failure, no pseudo tumors, no surface corrosion, no metallosis, etc. We have found the use of stem modularity to be safe and effective in the use in Primary Total Hip Arthroplasty.[14]
Key Words: modularity, neck, fatigue failure, pseudo tumors, corrosion, metallosis
* Co-Director, The Spine and Orthopedic Institute
St. Vincent Charity Medical Center, Cleveland Ohio
** Executive Director, JISRF, Chagrin Falls Ohio |
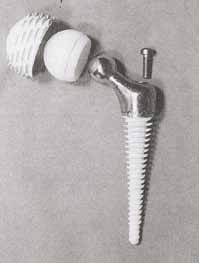
 S-Rom® Stem
S-Rom® Stem |
Introduction:
Modularity or multi-piece stems are becoming commonplace in hip revision surgery[12], with virtually all implant companies offering one version or another. The role of modularity would therefore seem to be firmly established for revision, but what of primary cases?[14]
This study is a follow-up to previous work with a further six years of cases reviewed. The real question we face, does the benefit of modularity pay higher dividends than the potential risk factors. We believe this review will provide guidance for other surgeons to aid in their decision making process.
For 26 years the senior author has collaborated with the co-author on proximal modularity in THA. The initial clinical work started in 1986 with the S-Rom® Modular Stem and has progressed over the past twenty six years to include three different stems styles and two different modular junctions: Dual Press[11,32] and Apex ARC™Neck Stabilized Stem[16,17]
 A screw anchored
A screw anchored
intramedullary hip stem
1978 Bousquet Design |
Modular Stem History
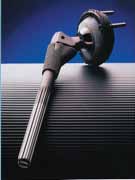
Modular stems have a long history starting with McBride in 1948 that utilized a threaded femoral component and publishing his first account in
JBJS in 1952. This was followed in 1978 by Bousquet and Bornand with the development of a proximal modular stem that featured a proximal body that was attached to a stem via a conical mounting post, with 8 perforations that allowed for select angle orientation for biomechanical restoration. Their design also featured a screw-anchored intramedullary stem design that was coated with AL2O3. Their initial reports were presented in Basel in June 1982 at a symposium on cementless hips and published in Morscher's 1984 book "The Cementless Fixation of Hip Endoprostheses". The BSP Modular stem followed in 1988 and featured a modular collar/neck assembly that was fixed to the stem with a morse taper joint, a saw-tooth macro interlock system (15º rotation per tooth) and a set screw.[18]
The current S-Rom® Stem System represents the fourth generation in the evolution of the Sivash Total Hip Stem since it was introduced in the United States in 1972.[16,22,23]
Sivash began development of his prosthesis in 1956 at the Central Institute for Orthopaedics and Traumatology, Moscow, Russia. By 1967 Sivash had selected titanium alloy for the femoral stem and proximal sleeve and chrome cobalt alloy for his socket bearing and femoral head. A major focus was the design of a constrained socket. The Sivash Total Hip System, introduced by the US Surgical Corporation, never received major clinical or market success, partially due to the difficulty of the surgical technique, and positioning of this constrained device.
S-Rom® Evolution
 S-Rom is virtually unchanged since 1986
S-Rom is virtually unchanged since 1986
|

Concerns with the S-Rom® Stem
Would modularity (stem-sleeve) produce fretting leading to osteolysis, and/or component failure?
 |
 S-Rom Grooved Style had a polished stem with a vertical groove & locking pin. The groove acted as a funnel for migration of poly debris causing distal bone lysis. S-Rom Grooved Style had a polished stem with a vertical groove & locking pin. The groove acted as a funnel for migration of poly debris causing distal bone lysis. |
S-Rom grooved style stem progressive osteolysis C. Engh. Groove in the stem allowed migration of debris. Resulting in a stem design change.

Cameron: Porous sleeve failed to in-grow, resulting in migration of poly debris.
Example of a fatigue failure in a young 37 yo male 85kg / failed at 4 years (W. Walter)
60 yo male failed at 12 years (W. Walter)
There have been a number of reported failures over the years however, the benefits of this stem design has offered significant advantages over the limited reported complications.[1,29,30]
Examples of Modular Site Failures[19,20,21,22,23,24,25,26,27,28,31]
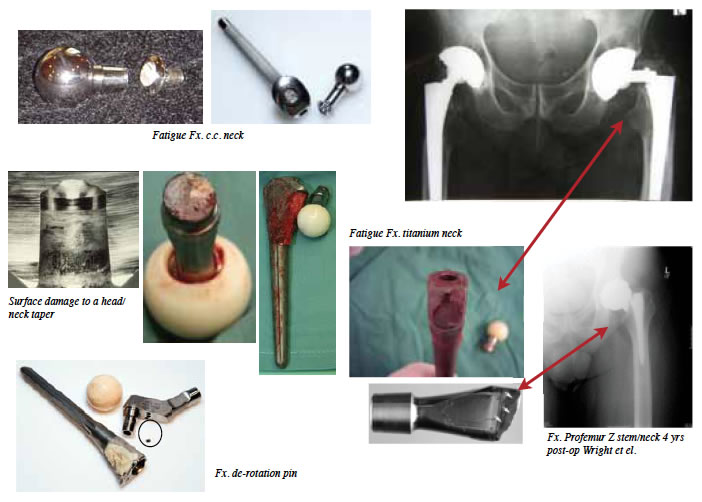
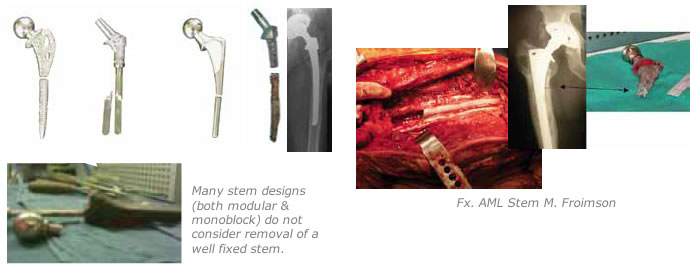
Many modular stem designs have come and gone.

It is important to understand why some of these designs failed to survive in the market place. All modular junctions are not equal in design and or function. |
 |
To be fair to modularity, monoblock stems have also met with their own problems.
Stress patterns as described by Bechtol[13]
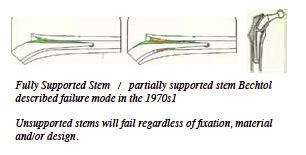 Fully Supported Stem / partially supported stem Bechtol described failure mode in the 1970s[1] Fully Supported Stem / partially supported stem Bechtol described failure mode in the 1970s[1]
Unsupported stems will fail regardless of fixation, material and/or design.
Modular junctions come in a variety of designs from femoral heads, neck taper sleeves, proximal modular necks, shoulders, metaphyseal sleeves, mid-stem tapers, mid-stem geared non-taper junctions and distal sleeves. Many have adjustable features; anteversion, retroversion at this junction. We continue to have the head-neck adjustment for length and many of these designs incorporate proximal segments with variable “offset” options.
While widely used and accepted in the revision stem market, the more extensive modularity is experiencing some problems in the primary market. The incidence of dislocation of primary hip replacement is quite variable but remains a signifi cant problem. A number of factors have resulted in a decrease risk of dislocation including smaller and improved neck designs, greater head to neck ratio, greater surgical options for leg length, femoral offset, soft tissue solutions such as repairing the capsule and increased popularity of the anterior approach.
Clearly however, implant malposition remains a primary cause of recurrent hip instability.[23]
Materials and Methods
From 1986 to May 2012 a total of 1,114 modular stems have been implanted for primary THA by the senior author.
- S-Rom® Stem (DePuy) = 537
- Apex Modular™ Stem (Omnilife) = 116
- Apex K2 Modular™ Stem (Omnilife) = 341
- Apex ARC™ Stem (Omnilife) = 120
All stems implanted by the same surgeon utilizing the posterior surgical approach. All the femoral stems are manufactured from titanium alloy (ASTM F136).
All acetabular components were cementless porous coated of a variety of designs and bearing surfaces. The acetabular cups in this series is not part of this review process.
Dual Press™ Modular Junction
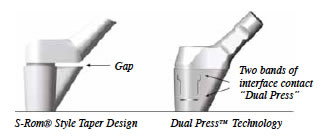 The femoral neck attaches to the body of the stem through a unique Dual Press™ connection that is simple, robust, and very stable. This modular design allows a large selection of necks, enabling the proper combination of anteversion angle, lateral offset, and neck length/leg length, to restore proper soft tissue tension and joint biomechanics. The femoral neck attaches to the body of the stem through a unique Dual Press™ connection that is simple, robust, and very stable. This modular design allows a large selection of necks, enabling the proper combination of anteversion angle, lateral offset, and neck length/leg length, to restore proper soft tissue tension and joint biomechanics.
S-Rom style modular junction is that of a taper between the stem body and internal portion of the sleeve.
 The Apex Modular™ Stem is the shape of a S-Rom style stem consisting of a circular fl uted distal stem with a proximal cone and medial triangle. The difference is in the ability to independently choose stem size, neck offset, version angles, and head size. The Apex Modular™ system allows surgeons to precisely address patient specifi c anatomical needs to achieve accurate leg length and soft tissue balance with the proximal neck/shoulder modularity. The proximal end of each stem includes an alignment pin that engages with the mating hole on the distal surface of each neck. Neutral necks have a single hole; anteversion necks have two holes for +/- 13° . This ability to adjust neck orientation eliminates the need for separate left and right stems, thus reducing inventory requirements, while enabling better restoration of joint biomechanics. The pin and hole also provide additional torsional stability, as well as control of the version angle. The Apex Modular™ Stem is the shape of a S-Rom style stem consisting of a circular fl uted distal stem with a proximal cone and medial triangle. The difference is in the ability to independently choose stem size, neck offset, version angles, and head size. The Apex Modular™ system allows surgeons to precisely address patient specifi c anatomical needs to achieve accurate leg length and soft tissue balance with the proximal neck/shoulder modularity. The proximal end of each stem includes an alignment pin that engages with the mating hole on the distal surface of each neck. Neutral necks have a single hole; anteversion necks have two holes for +/- 13° . This ability to adjust neck orientation eliminates the need for separate left and right stems, thus reducing inventory requirements, while enabling better restoration of joint biomechanics. The pin and hole also provide additional torsional stability, as well as control of the version angle.

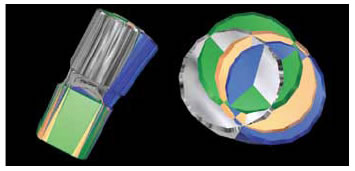
The K2 stem builds on the philosophy of a dualtapered trapezoidal stem geometry that facilitates primary fi xation and rotational stability. A straight forward and effi cient broach-only surgical technique is intended to preserve endosteal bone and intramedullary vascularization.
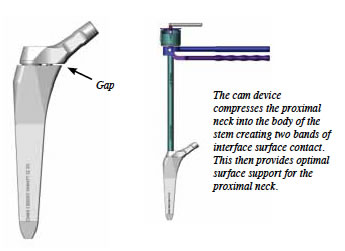 |
The cam device compresses the proximal neck into the body of the stem creating two bands of interface surface contact. This then provides optimal surface support for the proximal neck. |
 |
The ARC™ Neck Sparing Implant saves bone in Gruen zones 1,3,4,5 & 7 |
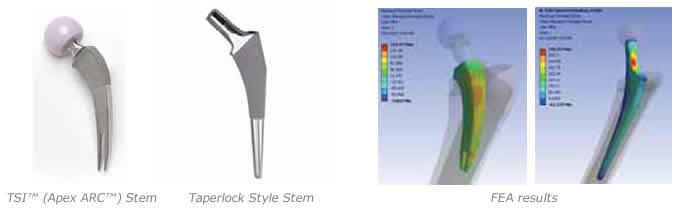
The Apex ARC™ Stem is licensed technology from Concept Design & Development™, LLC, Chagrin Falls, Ohio.
The Apex ARC hip system provides surgeons with the bone and soft tissue conserving benefi ts without the disadvantages of hip resurfacing, or metal-onmetal articulation, or a steep learning curve, or limited indications.
This stem can utilize any standard surgical approach including the direct single anterior incision or MIS approach.
The modular neck junction is a standard 12/14 Euro taper (ASTM standard for the Cone is size N listed as 5º 40’, +2.5’ -0’ or 5º 40 minutes + 2.5 minutes, -0 minutes.) So the surgeon can choose the bearing material best suited for the individual patient.
Note: Not all 12/14 tapers are equal (variants do exist) companies cannot recommend mixing and matching of different companies product. If you mix and match (off label use) make sure head / neck tapers are compatible.

Note: The simplest way to look at compatibility is to ask does the company use ASTM standard for size N taper?
The modular necks are available in neutral standard, long, 8º varus/valgus
standard,
8º varus/valgus long, 12º varus/valgus, & 12º anteverted/retroverted.
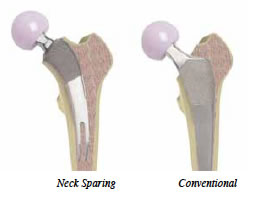 The design of the Apex ARC hip stem requires less bone to be removed during surgery, provides the opportunity for surgeons to dissect fewer soft tissues, and loads the proximal femur in such as a way as to provide an environment where bone could be preserved over time. The design of the Apex ARC hip stem requires less bone to be removed during surgery, provides the opportunity for surgeons to dissect fewer soft tissues, and loads the proximal femur in such as a way as to provide an environment where bone could be preserved over time.
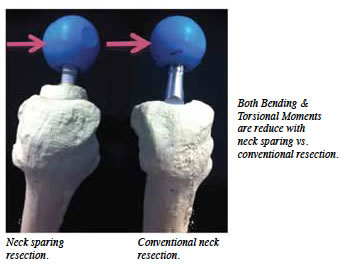
Finite Element Analysis comparing the TSI™ neck sparing design to a Taperlock style stem demonstrated the maximum principal tensile stress in the neck stabilization stem was 35% less than that of the monoblock Taperlock style design.[33]
Results
S-Rom
- Modular junction failures = 0
- Dislocations = 6 total (3 closed reductions, 3 open constrained sockets)
 |
Painful S-Rom stem required on-lay strut grafting |
Stem Revisions
- 4 total (0 for aseptic loosening, 4 late sepsis)
Painful Hip
- 5 pts: Required on-lay grafting for signifi cant progressive end of stem pain.
Painful S-Rom stem required on-lay strut grafting
Apex Modular & Apex K2 Stem
- Modular junction failures = 0
- Dislocations = 3 (Two patients with MoM bearings have had cup revision due to cup spin out. One patient was one (1) year out with an ASR metal acetabular component. Patient presented with increasing groin and buttock pain. X-rays demonstrated that original cup position had changed and did not appear to be ingrown. The proximal modular junction of the K2 stem was disengaged allowing access to the socket. K2 removal instruments provide ease of removal of proximal modular body making cup revision signifi cantly easier with less bone destruction.
K2 Dual Press removal instrument
 |
Explanted cup |
The Explant cup removal system (Zimmer) was used making removal with minimal bone loss possible.
A cementless porous component with adjunct screw and poly bearing was then inserted.
 |
|
|
MoM cup spinout |
|
Revised with new cup & neck neck |
Second patient was female that presented a spun out MoM (Wright Medical) acetabular bearing component at her fi rst post-op visit at seven (7) weeks. Since intra-operative x-rays are taken on all patients it is assumed that cup slippage accrued during the early post-op period and then stabilized. Again the proximal modular junction was disengaged and cup removed with Explant system.
 A new proximal modular neck and head were implanted with a cementless porous cup with one (1) screw for adjunct fi xation. A new proximal modular neck and head were implanted with a cementless porous cup with one (1) screw for adjunct fi xation.
One additional patient had multiple dislocations and was revised by disengagement of the proximal modular junction and exchanged with an increased femoral offset and anterverted modular neck.
- Leg/length discrepancy +/- 7mm = 0
- Aseptic loosening = 0
- Stem Revisions = 0
- Modular neck exchanges = 3
The third neck exchange was for a patient that had a 36 mm metal on poly bearing that met with multiple dislocations. Patient was treated with proximal neck exchanged to an increased femoral offset and anteverted position.
The Apex ARC™ Neck Sparing Stem
- Modular junction failures = 0
- Stem revisions = 2
 |
Explanted stem |
One stem removed for sepsis.
One removed for traumatic dislocation, converted to an Apex Modular Primary stem.
Female with a posterior dislocation poly exchanged from neutral liner to a 15º and an increase in 3.5 mm vertical height neck position into max 12º varus position.
Note: At the time of surgery a large soft tissue mass was found anteriorly and was thought to be associated with bowstringing of the anterior superior capsule as an unusual consequence of the posterior capsular repair.
The second case removed the neck for access to the socket (cup & poly replaced along with a new neck).

Poly Exchange |
|
 |
Explanted head, neck & poly |
Both cases had reduced operating room time since the modular junctions functioned as designed. Proximal modularity allows access for revisions situations reducing overall complications associated with stem removal and increased operating time.
- Intraoperative calcar cracks = 2 Small chip fractures not treated.
- Intraoperative calcar cracks resulting in stem bail out = 2
Both occurred in small female patients where the size 1 stem was too large. Both revisions were converted to primary Apex Modular stem. Since the introduction of the size 0 stem we have not had to bail out of any routine primary cases.
- Aseptic Loosening = 0
- Leg Length Discrepancy +/- 7mm = 0
- Subsidence >5mm = 0
 |
ARC™ Stem Size 1 vs. 0 |
Currently the short curved ARC™ Neck Sparing Stem is used as my primary total hip stem in all Dorr bone classifi cations (A, B, & C). Patient range from mid twenties to mid eighties.
In the smaller female patient, if we cannot get to a 32mm head diameter we will use a Dual Mobile Style Cup. We have used two different styles: One an anatomical style by Stryker and a hemispherical style by Omnilife.
The introduction of the smaller size 0 stem has eliminated the risk of trying to overstuff a size 1 stem into a smaller femoral neck. Overall size is reduced along with elimination of the lateral T-Back.
The Anteverted / Retroverted (12º) neck has been added to aid in addressing combined version angles and reduces potential mechanical impingement issues.

Modular necks available in different orientations: Neutral, regular & long, 8º varus / valgus regular & long, 12º varus / valgus & 12º anteverted /retroverted |

1986 S-Rom 2010 ARC™ Stem |
Observations & Summary
In over 1,114 primary cementless total hip arthroplasties performed by the same surgeon in two community hospitals over 26 years, there has never been a related modular junction failure. There have been no signs of pseudo tumors, surface corrosion, metallosis, etc.
I still use the S-Rom® stem for CDH and revision surgery. In Dorr type A Bone, I will select the Apex Modular™ stem. In type C Bone, if I don’t believe I can get a solid lock in the neck, I will use the K2 Trapezoid Modular Stem. For all my routine OA cases I am using the Apex ARC™ Short Curved Neck Sparing Stem.
It is not unusual for me to use two or three different modular stems in any given surgical day.
I have met with problems with bearing materials, acetabular components and periprosthetic fractures. However, when it comes to modularity, I have been very selective on the modular junctions that I have used and have found them to be of signifi cant advantage in my clinical / surgical practice. I take intraoperative x-rays on every case and alter my selection of components on average 70% of the time.
All modular junctions are not equal in design and performance. It is critical to understand the design limitations and required surgical techniques to ensure proper performance of modular total hip arthroplasty.
The newer short curved neck sparing stem design has reduced my O.R. time by 15-20 minutes by use of the femur fi rst surgical technique. There appears to be less blood loss and patients are back to full activities quicker.
The advancements of modularity has proven to be benefi cial to my practice.
I am aware of the concerns regarding modular junctions and will continue to monitor my patients and report on my experience every few years.
References
- Patel A, Bliss J, Calfee R, Froehlich J, Limbird R; Modular femoral stem-sleeve junction failure after primary total hip arthroplasty. J of Arthroplasty, Vol. 24, issue 7, Oct. 2009
- Bobyn J, Tanzer M, Krygier J, et al. Concerns with modularity in total hip arthroplasty. Clin Orthop. 1994;298:27
- Viceconti M, Baleani M, Squarzoni S, et al. fretting wear in a modular neck hip prosthesis. J Biomed Mater Res. 1997;35:207
- Collier J, Supernant V, Jensen R, et al. Corrosion between the components of modular femoral hip prostheses. J Bone Joint Surg. 1992;74B:511
- Gilbert J, Buckley C, Jacobs J; In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations: the effects of stress motion and alloy coupling. J Biomed Mater Res. 1993;27:1533
- Cook S, Barrack R, Clemow A. Corrosion and wear at the modular interface of uncemented femoral stems. J Bone Joint Surg Br. 1994;76:68
- Fontana MG, Greene ND. Corrosion Engineering. 3rd ed. New York: McGraw-Hill; 1986;
- Christie M, DeBoer D, Trick L, et al. Primary total hip arthroplasty with use of the modular S-ROM prosthesis. Four to seven-year clinical and radiographic results. J Bone Joint Surg Am. 1999;81:1707
- Krygier J, Dujovne , Bobyn J. Fatigue behaviour of titanium femoral hip prosthesis with proximal sleeve stem modularity. J Appl Biomaterials. 1994;5:195
- Cook S, Manely M, Kester M, et al. Torsional resistance modular sleeve-stem hip system. Clin Mater. 1993;12:153
- Cheal E, Cipolletti G. Assembly, fatigue and fretting resistance of the Apex modular hip stem. Apex surgical web site.
- McTighe T, Cameron H, Keppler L, Tkach T. Historical Review of Stem Modularity. Ref Book on Total Hip Modularity, JISRF Pub Third Edition 2009 www.jisrf.org
- Bechtol, C.O.: “Failure of Femoral Implant Components In Total Hip Replacement Operations” Ortho Rev. Vol. IV, No. 11, Nov.1975
- Keppler L, Cameron H, McTighe T, The Role of Modularity in Primary THA-Is There One?, AAOS Scientific Exhibit 2006 / www.jisrf.org
- Cameron H, Jung Y, Noiles D, McTighe, T. “Design Features and Early Proximally Fixed Low Bending Stiffness Uncemented Total Hip Replacement” AAOS Scientific Exhibit 1988 /www.jisrf.org
- McTighe T, Woodgate I, Turnbull A, Keggi J, Kennon R, Keppler L, et al. A New Approach to neck Sparing THA Stem, AAOS poster exhibit 32 2008 / www.jisrf.org
- McTighe T, Woodgate I, Turnbull A, Harrison J, Keggi J, Keppler L, et al. A New Approach to Neck sparing THA Stem, oral paper Arthroplasty Society of Australia Scientific Meeting, May 2008
- Bousquet G, Bornard F. “A Screw-Anchored Intramedullary Hip Prosthesis” 1984 Morscher Book pages 242-246 Springer-Verlag Cementless Fixation of Hip Endoprostheses”
- Bobyn J, Collier J, Mayor M, McTighe T, Tanzer M, Vaughn B. Particulate Debris in Total Hip Arthroplasty: Problems and Solutions, AAOS Scientific Exhibit 1993 / www.jisrf.org
- Collier J, Surprenant V, Jensen R, Mayor M. Corrosion at the interface of cobalt-alloy heads on titanium-alloy stems. Clin. Orthop. 271:305.1991
- Dujove A, Bobyn J, Krygier J, et al. Fretting at the head/neck taper of modular hip protheses: Tran. of 4th World Bionnat. Congress, Berlin, 1992, p.264
- Wright G, Sporer S, Urban R, Jacobs J. Fracture of a Modular Femoral Neck After Total Hip Arthroplasty, A Case Report J Bone Joint Surg Am. 2010 June; 92(6): 1518–1521. doi: 10.2106/JBJS.I.01033
- Callanan M, Bryan J, Bragdon C, Zurakowski D, Rubash H. Risk Factors in Cup Malpositioning, John Charnley Award 2010 Hip Society
- Stryker Field Safety Notice RA2012-067 ABGII Modular Stems and ABGII Modular Necks Rejuvenate Modular Stems and Rejuvenate Modular Necks; Issue: This communication is intended to inform implanting and/or treating surgeons and other healthcare professionals that Stryker has updated the Instructions for Use (IFU) for the ABGII Modular and Rejuvenate Modular Hip Systems. This is based on a reported rate of less than one percent for revisions potentially associated with fretting and/or corrosion at or about the modular neck junction.
- Heim C, Postak P, Greenwald S. Femoral Stem Fatigue Characteristics Of Modular Hip Designs - Series II, AAOS Scientific Exhibit 1995, Orthopaedic Research Laboratories The Mt. Sinai Medical Center
- Froehlich J, McTighe T, Cameron H, Keggi K, Keggi J, Kennon R, Woodgate I. Defining The Role Of Modular Stem Designs In THA, Poster Oct. 2006 ISTA / www.jisrf.org
- Keggi K, Keggi J, Kennon R, Tkach T, Low W, Froehlich J, McTighe T, Cheal E, Cipolletti G. “Within Any Important Issue, There Are Always Aspects No One Wishes To Discuss” – Femoral Component Failure; Poster 2006 ISTA Meeting, www.jisrf.org
- Srinivasan A, Jung E, Levine B. Modularity of the Femoral Component in Total Hip Arthroplasty, J Am Acad Orthop Surg April 2012 vol. 20 no. 4 214-222
- Buly R. The S-ROM Stem: Versatility of Stem/Sleeve Combinations and Head Options; Sept. 11, 2005 Orthopaedics Today
- Lim S, Moon YW, Eun SS. Total Hip Arthroplasty Using the S-Rom Modular Stem After Joint-Preserving Procedures for Osteonecrosis of the Femoral head, J. of Arthroplasty Vol. 23 No. 4 2008
- Carlson J, Van Citters D, Currier J, Bryant A, Mayor M, Collier J. Femoral Stem Fracture and In Vivo Corrosion of Retrieve Modular Femoral Hips, The Journal of Arthroplasty Available online 28
December 2011
- Keggi K, Keggi J, Kennon R, Keppler L, Turnbull A, McTighe T. Proximal Modular Stem Design “Dual Press™” With a Dual-Tapered “K2™” Trapezoid Stems, JISRF pub Feb. 2009 / www.jisrf.org
- Brazil D, McTighe T, FEA Analysis of Neck Sparing vs Conventional Cementless Stem, Vol. 1, 1, Reconstructive Review October 31, 2011
|

